Folic Acid Side Effects
Hardly anyone talks about folic acid side effects.
Folic acid is not some major block buster drug having a list of dangerous side effects longer than its benefits.
Like all the ones on TV….
According to WebMD, folic acid effects are these:
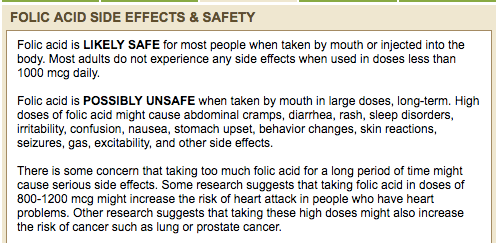
While these are great to know, these are not the folic acid side effects I want to share with you.
I want to inform you about the ‘hidden’ or ‘undiscussed’ side effects of folic acid.
Note: All published references supporting my presentation are below – at the bottom of this article.
Why is no one talking about what I am about to show you?
Likely because you have to really, really – REALLY – dig for them.
Published literature contains very little on the side effects of folic acid.
In fact, using that term won’t get you much.
Instead of searching for ‘folic acid side effects’ to get you the information you want, you need to be creative.
Let’s walk through this step by step.
It will be worth your while…
MTHFR testing has exploded globally.
The positive finding is triggering a flurry of L-5-MTHF supplementation or prescriptive medication. This is the inappropriate response. MTHFR variants have been present for countless generations.
The increase in cardiovascular diseases, congenital birth defects, infertility, recurrent miscarriages are NOT a result of the MTHFR variant.
It is a result of the environmental impact on MTHFR expression.
MTHFR is unable to handle the current present-day load.
A big factor weighing down MTHFR:
Folic acid.
Whole Food to Processed Food
Plants grew and provided natural forms of folate. We harvested the fresh plants and utilized them immediately in various ways. Salads, steamed, dried, baked. In this manner, we received the nutrients as offered by the plant itself. One such nutrient provided by plants – especially leafy greens – is folate.
Folate comes from the Latin root ‘folium, which means leaf.
This powerful nutrient provides one of the most fundamentally important compounds in human biochemistry – the methyl group.
Access to these foods changed during the industrialized era. Instead of fresh breads baked daily, big business looked for ways to mass produce. The issue with mass production of finished food products, such as bread, was shelf life. It was found that if the outer parts of the grains were stripped off and milled, shelf life was extended dramatically.
The result of extended shelf life led to a surge in production and profits. It also led to a surge in birth defects and medical issues.
The Rise of Folic Acid
Instead of fixing the solution by reverting back to whole grains and fresh food, an artificial nutrient was created and added to these processed foods.
Folic acid.
In the rush to get folic acid to market, it was tested only on rats. It turns out that rats have a high ability to convert folic acid into a more bioavailable form of folate – dihydrofolate.
We are not using folic acid in rats. We are using it in humans.
This synthetic nutrient has indeed proven to reduce some incidences of birth defects and signs of folate deficiency.
It hasn’t done it successfully enough.
What we are finding now is that folic acid is actually harming us.
Folic acid is doing it quietly and insidiously.
Folic Acid: It’s Not the Same
Folic acid has no known physiological effect on human biochemistry.
Zero.
While folic acid looks similar to natural folate, it is not close enough. Synthetic folic acid is lacking the body’s most fundamental biochemical compound – a methyl group.
To convert folic acid into methylated folate requires a) multiple functional genes producing b) functional enzymes which requires c) adequate cofactors. This is difficult enough. It is not all. The enzymes produced must also be in an environment free of compounds which interfere with their function – such as medications, heavy metals, cytokines, chemicals.
While rats can convert folic acid into dihydrofolate quickly and successfully, human biochemistry does not.
Only 200 mcg of folic acid can move through a human enzyme called DHFR. This is in humans who have a functional DHFR gene. There are known DHFR variants which lead to a further significant reduction in function. What does this mean? It means that folic acid is even less effective.
We made a dangerous assumption. We assumed since rats can convert folic acid easily into dihydrofolate, humans can too.
Since humans cannot convert folic acid effectively, the excess leads to high amounts of what is known as unmetabolized folic acid in the blood. Unmetabolized folic acid is folic acid.
Unmetabolized Folic Acid: It’s Harmful
Here are the reasons why unmetabolized folic acid is harmful:
- Has no physiological benefit to the host until it is converted into dihydrofolate
- Folate transport proteins bind it preferentially over more reduced active folate
- Folate receptors bind it preferentially over more reduced active folate
- Contributes to a pseudo MTHFR deficiency due to enzymatic inhibition of MTHFR
- Reduces DHFR enzymatic function which reduces biopterin recycling, thereby contributing to a biopterin deficiency
- Masks a vitamin B12 deficiency
This combination of negative physiological effects of folic acid is extremely significant.
In sum, they lead to what is called a ‘functional folate deficiency.’
Determining a Folate Deficiency
Common labs which measure serum folate are measuring the entire folate pool in the blood.
One cannot assume that serum folate contains the most active form of folate – which it should. Over 80% of circulating folate should be L-5-methyltetrahydrofolate. This is far from what many individuals have circulating.
Serum folate consists of unmetabolized folic acid, dihydrofolate, tetrahydrofolate, folinic acid, L-5-MTHF. This is not clinically useful information except only in the case of frank folate deficiency when serum folate is low.
The only ways to determine a functional folate deficiency:
- History: “How much folic acid are you taking?” and “How much processed food are you eating? (as folic acid is found in these)
- Lab: Measuring ‘UMFA’ which is unmetabolized folic acid. Issue is labs do not measure this. They used to but stopped due to lack of demand. We need it back.
- Lab: Measuring Cerebral folate which is quite invasive.
If cerebral folate deficiency is identified, prescribing folic acid to treat it is . . . contraindicated.
Yes.
Folic acid is a known contraindication of cerebral folate deficiency.
This alone begs the question:
Why are we using folic acid at all?
Couldn’t we all be struggling with some level of cerebral folate deficiency?
Folate: It’s what we need
Folic acid served its purpose.
Industrialization stripped grains of natural vitamins, oils and fiber. This led to a dramatic increase in miscarriages and birth defects. Governments had to do something. The solution chosen was not to revert back to using whole grains; it was to use synthetic man-made folic acid which has no physiological effect until it is metabolized into more reduced folates.
The use of folic acid absolutely did reduce the incidence of miscarriages and birth defects – in some. Not nearly enough especially in Hispanic populations.
The FDA is working on fortifying corn flour now with folic acid.
This is not the solution.
The solution is to use natural forms of folate which are readily available and nearly as inexpensive as folic acid.
Without the presence of folic acid, natural folates may:
- Bind to folate transport proteins freely
- Bind to folate receptors freely
- Help synthesize biopterin
- Not mask a vitamin B12 deficiency
- Enhance cellular folate levels
Fixing the Folate Problem
Folic acid is mandated to be included in many processed foods by many countries around the world. Stopping this bad practice is not going to cease any time soon.
Thankfully, steps may be taken right now to optimize human folate levels:
- Avoid processed foods containing synthetic folic acid
- Consume whole foods containing natural folates
- Avoid supplements containing folic acid.
- Utilize supplements containing folinic acid (calcium folinate) and/or L-Methylfolate (aka L-5-MTHF, 6S-5-MTHF)
- Consume organ meats such as liver (grass fed, younger animals)
While the above steps will indeed support one’s folate levels, it is not sufficient enough to make a difference across the globe.
Education.
This is what needs to happen now in order to reduce the risks of functional folate deficiency.
How You Can Help
Now that you are aware of the potential risks of folic acid, you can now reduce your risk of functional folate deficiency.
Ways you can help protect others from functional folate deficiency:
- Pass this article on. Share it.
- At health food stores, talk with the manager of the vitamin section and let them know the risks of folic acid. They will listen to you.
- At your doctor, talk with them about the difference between folic acid and folate. Some will listen and some won’t. Even if one listens, you are making a difference.
- At supplement stores, talk with the manager about the differences between folate and folic acid. Many want to be on the cutting edge and will appreciate your information.
Additional resources:
- DrBenLynch.com – Access Dr Lynch’s ’26 Ways to Clean Your Genes’ which is a Free Bonus Chapter. You may also learn more from Dr. Ben Lynch via his YouTube, Facebook Live, Articles and Podcasts.
- Dirty Genes: A Breakthrough Program to Treat the Root Cause of Illness and Optimize Your Health. This book summarizes how folic acid, and many other things, contribute to reducing the function of our genes and thus our health.
Share your story about Folic Acid Side Effects below.
Leave a comment.
Over the many years I’ve talked about this, I know many who have benefitted greatly from eliminating folic acid from their diet.
Are you one of them?
References
[1] Pfeiffer CM, Sternberg MR, Fazili Z, Yetley EA. Lacher DA, Bailey RL, Johnson CL. Unmetabolized folic acid is detected in nearly all serum samples from US children, adolescents, and adults. The Journal of Nutrition. 2015 Mar;145(3):520–31. PubMed PMID: 2573468.
[2] Kalmbach RD, Choumenkovitch SF, Troen AP, Jacques PF, D’Agostino R, Selhub J. A 19-Base Pair Deletion Polymorphism in Dihydrofolate Reductase Is Associated with Increased Unmetabolized Folic Acid in Plasma and Decreased Red Blood Cell Folate. The Journal of Nutrition. 2008 Dec;138(12). PubMed PMID: 19022952.
[3] Bailey SW, Ailing, JE. The extremely slow and variable activity of dihydrofolate reductase in human liver and its implications for high folic acid intake. Proceedings of the National Academy of the Sciences of the United States of America. 2009 Sep 8;106(36). PubMed PMID: 19706381.
[4] What are single nucleotide polymorphisms (SNPs)? Genetics Home Reference. 2017 Oct. https://ghr.nlm.nih.gov/primer/genomicresearch/snp.
[5] Kes VB, Jurasic MJ, Zavoreo I, Coric L, Rotim K. Migraine, carotid stiffness and genetic polymorphism. Acta Clinica Croatica. 2015 Dec;54(4):409–16. PubMed PMID: 27017713.
[6] Li C, Yichao J, Jiaxin L, Yueting Z, Qin L, Tonghua Y. Methlylenetetrahydrofolate reductase gene polymorphism and risk of chronic myelogenous leukemia: a meta-analysis. Journal of B.U.ON: official journal of the Balkan Union of Oncology. 2015 Nov-Dec;20(6):1534–45. PubMed PMID: 26854451.
[7] Remuzgo-Martinez S, Genre F, Lopez-Rejias R, Ubilla B, Mijares V, Pina T, Corrales A, Blanco R, Martin J, Llorca J, Gonzalez-Gay MA. Decreased expression of methylene tetrahydrofolate reductase (MTHFR) gene in patients with rheumatoid arthrtis. Clinical and Experimental Rheumatology. 2016 Jan-Feb;34(1):106–10. PubMed PMID: 26843177.
[8] Strohle A, Bohn T. Folate and prevention of neural tube defects: new insights from a bayesian model. International Journal for Vitamin and Nutrition Research. 2015;85(3-4):109–11. PubMed PMID: 26780389.
[9] Yun L, Xu R, Li G, Yao Y, Li J, Cong D, Xu X, Zhang L. Homocysteine and the C677T gene polymorphism of its key metabolic enzyme MTHFR are risk factors of early renal damage in hypertension in a chinese han population. Medicine. 2015 Dec;94(52). PubMed PMID: 26717388.
[10] van der put MJ, Gabreels F, Stephens E, Smeitink J, Trijbels F, Eskes T, van den Heuvel L, Blom H. 1998;62:1044–1051.
[11] Strohle A, Bohn T. Folate and prevention of neural tube defects: new insights from a bayesian model. International Journal for Vitamin and Nutrition Research. 2015;85(3-4):109–11. PubMed PMID: 26780389.
[12] Smith AD, Kim YI, Refsum H. Is folic acid good for everyone? The American Journal of clinical nutrition. 2008 Mar;87(3):517–33. PubMed PMID: 18326588.
[13] Strickland KC, Krupenko NI, Krupenko SA. Molecular mechanisms underlying the potentially adverse effects of folate. Clinical chemistry and laboratory medicine. 2013 Mar 1;51(3):607–16. PubMed PMID: 23241610.
[14] Blom HJ, Shaw GM, den Heijer M, Finnell RH. Neural tube defects and folate: case far from closed. Nature Reviews. 2006 Sep 7(9):724-31. PubMed PMID: 16924261.
[15] Hyland K, Shoffner J, Heales SJ. Cerebral folate deficiency. Journal of Inherited Metabolic Disease. 2010 Oct;33(5):563–70. PubMed PMID: 20668945.
[16] Prinz-Langenohl R, Bramswig S, Tobolski O, Smulders YM, Smith DE, Finglas PM, Pietrzik K. [6S]-5-methyltetrahydrofolate increases plasma folate more effectively than folic acid in women with the homozygous or wild-type 677C–>T polymorphism of methylenetetrahydrofolate reductase. British Journal of Pharmacology. 2009 Dec;158(8):2014–21. PubMed PMID: 19907061.
[17] Greenberg JA, Bell SJ. Multivitamin Supplementation During Pregnancy: Emphasis on Folic Acid and l-Methylfolate. Reviews in Obstretics and Gynocology. 2011;4(3-4):126–7. PubMed PMID: 22229066.
[18] Obeid R, Holzgreve W, Pietrzik K. Is 5-methyltetrahydrofolate an alternative to folic acid for the prevention of neural tube defects? Journal of Perinatal Medicine. 2013 Sep 1;41(5):469–83. PubMed PMID: 23482308.
 800-470-7401
800-470-7401
7 Comments
What I’m taking from all I’ve read here is that natural forms such as liver, broccoli, etc are better forms of getting folate and methyl folate should be taken and not just folate for MTHFR deficiency? Is this available over the counter? Would supplementing diet with the above foods be enough without having to consume a pill? The only thing I would have a problem with is liver. My mom used to give it to us regularly as a twice a week dinner with lots of veges. It made me nauseated to eat it and I don’t like it. Maybe cooking it with onions would help?
Thank you for this informative article. I would like to see more.
NML
I am homozygous for MTHFR. If I consume folic acid, it makes me incredibly sick. I become severely agitated, I have chills (but no fever). This is not your run of the mill angry mommy agitated. This is panic attack, drug withdrawal, crazed animal agitation. It is horrible. It lead to severe anxiety and depression and literally years of near constant suicidal ideation because I was in this kind of mental turmoil so frequently and without any obvious cause. I was never on psych meds because I also have ptsd and do all my treatment was behavioral therapy of one kind or another. So I suffered undiagnosed for most of my adult before I finally found a psychiatrist who diagnosed it in my mid 30s.
The MTHFR diagnosis was a game changer. I stopped consuming FA and started taking methylfolate daily. Within 24 my life was completely changed. I’m not kidding. The depression, anxiety, interminable panic attacks all disappeared because my brain was no longer chronically inflamed. I no longer had dementia quality brain fog either.
It pains me to think of all the people out there suffering from psychological problems that may be nutritional and brought about by an artificial substance mandated to be added to food by governments and touted as completely safe by the cdc. It nearly destroyed my life.
And I wish I had more information on it as few doctors I’ve found struggle to really understand MTHFR and folic acid. I want to be able to read a blog that says “this is what a folic acid attack looks like”….
I am terribly sorry to hear of your experience, but yes, many people are still prescribed folic acid, not methyl folate. It is quite amazing what a difference TRUE folate can do. We hope that DrBenLynch.com blog articles can provide you with some great information and insight to this. You can also review MTHFR.net for more information.
I concur with the story above, although I have severe chronic migraine with auras of several kinds and Mast Cell Activation Syndrome, and Autonomic Dysfunction (diagnosed respectively 15 years,14 , and 22 learns later) rather than ptsd.
When I suspected Folic Acid and did quit it, my condition lifted WITHIN 24 HOURS!
no kidding.
I took FA for 4 years of living hell to “force iron into my system” – other Fe tablets made no difference to my chronic anemia, related to the weakness-fatigue of ME/CFS.
The effect was a Serotonin toxicity syndrome (too much) of agitation so bad that every day I woke up wanting to die to make the torture stop, The doctor confused this for depression (low ST); wanted me in talk therapy (been there done that – never resolved the problem of ENERGY REGULATION); each drug tried gave terrible side-effects: until I said Enough – your “cure” is worse than the torture in my brain.
I also developped intolerances to pretty much everything, and auras became more frequent.
I would qualify that toxic state as in the post above: wildlife “crazed” behaviour under too much pressure (envirinmental and metabolic)… Only when it lasts for years, it destoys your entire life in society. I ended up homeless…. And blamed by everybody.
This is after the contraceptive pill as “treatment for acne” that never worked, destoyed my brain’s capacity for mathematics, and stole my career as a physicist.
Medical “doctors” and their drugs have GOT to stop taking children, girls, women for guinea pigs!
Please write for women on this pseudo-“depression” of agitation INDUCED BY SYNTHETIC FOLiC ACID.
I’ve just bought a multi vitamin that contains Folic Acid, I won’t be able to return it. It has 1,360 mcg DFE. I really don’t want to throw these away. Can I take it with your b vitamin complex, would that help off set the imbalance?
Dr. Lynch does not suggest folic acid, and actually writes and speaks on a lot of the dangers of taking it. It is not necessarily something you can “off set”. Read his book, Dirty Genes to find out more.
Thank you very good information and I love how you presented it. Humor with reality. and I will pass the info on. I hope to someday get the 23 and me and come see you to see what dirty genes are activated. I enjoyed listening to your audio book “Diety Genes”. Very well read and informative.