Does SIBO Affect Histamine Intolerance and DAO?
SIBO is a growing issue.
Risk increases with age and approximately 15% of those who are older struggle with SIBO. (source)
Why?
-
- Antacids
- Stress
- Lower stomach acid production
- Antibiotic overuse and resistance
- Methylation issues (leading to decreased bile production and bile flow)
- …. many more …
Histamine intolerance is also huge issue.
It is unknown how many struggle with histamine intolerance but I can tell you from experience – it is a TON of people.
Symptoms of histamine intolerance are vast and the treatments are often unknown or just suppressive at best.
The question is:
Is SIBO and Histamine Intolerance Linked?
When @DavidRockefeller tweeted @SeekingHealth this question, I had to respond:

What does this mean?
Let’s go step by step so you can see how bacteria in your small intestine contributes to full body histamine intolerance:
- Your small intestine is not supposed to have that much bacteria in it. It has defenses built in to prevent this from happening.
- Bacterial overgrowth in your small intestine may produce histamine. The bacteria themselves can produce histamine.
- The DAO enzyme, which resides in your small and large intestine, works hard to reduce the histamine from food, drink and bacteria.
- The DAO enzyme gets overwhelmed from all the histamine and cannot get rid of it all.
- The excess histamine contributes to gut dysfunction – including leaky gut, inflammation, food intolerance and altered bowel movements.
- The histamine in your digestive system gets absorbed into your blood and circulates throughout your entire body – including your brain, skin, heart, lungs, liver.
- Higher histamine in these organs and tissues leads to symptoms of headache and irritability (brain), red face, hot, sweaty, eczema, psoriasis and red lines if scratched (skin), increased heart rate (heart), difficulty breathing and asthma (lungs), increased utilization of methylation and nutrients which support methylation (liver).
- Even if the DAO enzyme works hard to start breaking down the histamine, if there are additional blockages in other enzymes, harmful levels of aldehydes will increase. Aldehydes are very toxic and lead to a vast number of symptoms. Vitamin B1, known as thiamine, is a big player help reduce aldehydes.
Wow, right?
Let’s look at step 1 and 2 more closely.
Your small intestine does have some bacteria in it – and it should. The most bacteria, though, should be in your colon.
“The density of bacteria increases from 100 bacteria in the proximal small intestine to 100,000,000 in the distal ileum, and 1,000,000,000,000 in the colon.” source
Bacterial overgrowth is kept at bay by natural small intestinal defenses.
“The epithelium of the small intestine is continuously in contact with food antigens, the enteric commensal bacteria, and potential pathogens that enter the host through the diet. The bacterial load in the small intestine is low and it increases distally. To keep the bacterial count low, the small intestine employs its motility to sweep bacteria along, mucus, and antibacterial molecules secreted in the gastric acid, biliary juice, as well as substances produced by the commensal microflora and epithelial cells, such as Paneth cells.” source
Summary:
The small intestine has built in defenses to keep bacterial overgrowth at bay.
If you have SIBO, then your defenses are down.
Restore your small intestinal defenses by:
- deep restful sleep
- stress reduction
- being calm while eating
- getting rid of antacids
- chewing your food
- going to the bathroom when you feel the urge vs suppressing it because it’s inconvenient
- eating when eating (no TV, phone, car, working) and being relaxed while doing so
- supporting your bile production with taurine and phosphatidylcholine
Is histamine really secreted during times of SIBO or gut infections?
Yes.
“[Testing] revealed the huge extent of inflammatory changes that are induced in the human intestinal epithelial cells when challenged by LPS and immune cells in combination on-chip, as both proinflammatory and antiinflammatory processes became activated. For instance, there was a dramatic up-regulation of receptors for histamine . . . as well as with clinical reports that show high levels of histamine routinely found in IBD patients.” (source)
Histamine levels are higher in those with LPS elevations. LPS, also known as endotoxin, is a chemical secreted by harmful bacteria. If one with SIBO have LPS-producing bacteria, then they will have high histamine levels which override their DAO enzyme.
“Our study provides the first direct evidence of role of SIBO and endotoxemia (LPS) and its relation with TLR signaling genes and liver histology in patients with non-alcoholic fatty liver.”
Parasitic infections, IBS, colitis, food allergies also contribute to higher histamine levels:
“Mastocytosis and presumably elevated availability of histamine are present in microscopic colitis, parasitic infections, IBS, and no doubt additional functional gastrointestinal disorders associated with symptoms of cramping abdominal pain, watery diarrhea, and defecation urgency.” (source)
Is histamine bad and something we have to fight?
No.
Histamine is useful to support immune balance and to eliminate pathogens.
“Mast cells (the cells which secrete histamine) also bridge communication between the immune and nervous systems by producing neurotransmitters and other mediators, such as NGF, serotonin, Substance P, and nitric oxide. In addition to inflammatory pain, mast cells to neuron communication likely contributes to processes, such as gut motility, that promote parasite expulsion.” source
Genetics of Histamine Intolerance
This is a major discussion and entails many genes and epigenetic factors.
Here is someone’s Histamine Pathway taken from StrateGene:
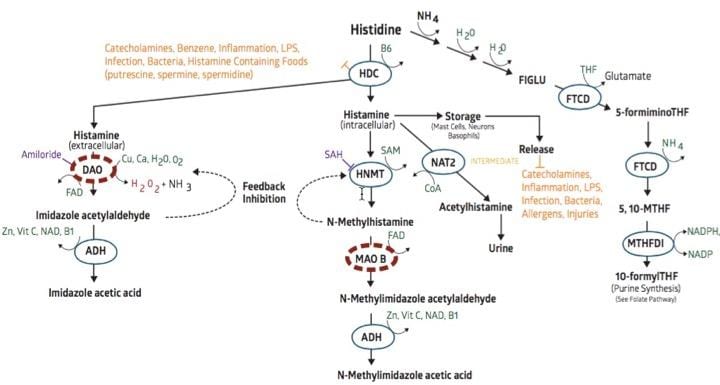
(note: 23andme v5 chip does not test for DAO SNPs currently. Prior chips do. If you did your 23andMe prior to August 2017, your raw data will have DAO information to run through StrateGene.)
As you can see, bacteria increase production of histamine by stimulating the HDC gene.
The DAO gene in this individual is slowed down with a known DAO genetic polymorphism.
This individual is more susceptible to histamine intolerance than one without SNPs in the DAO, NAT2 and MAOB genes.
We haven’t even looked at nutritional deficiencies which impact enzymatic function.
DAO needs copper and calcium in order to function. (source) (note: FAD is not needed – that is a different DAO gene and a typo we’re fixing).
DAO is also slowed down by the medications, Amiloride and Metformin.
Hydrogen peroxide (shown as H202) is given off when the DAO gene is working hard on your behalf. One needs ample glutathione in order to neutralize harmful hydrogen peroxide levels.
If histamine is processed by the DAO enzyme, the histamine becomes imidazole acetylaldehyde. This compound, if builds up, will feedback inhibit and slow down the DAO enzyme from working. This increases histamine levels and histamine intolerance.
Thus, in order to move imidazole acetylaldehyde out, one needs to have the ADH enzyme working well. This requires nutrients of zinc, vitamin C, vitamin B1 (thiamine) and vitamin B3 (niacin).
As you can see, it is not as simple as what SNP equals what supplement.
1 + 1 does NOT = 2 when it comes to genetic testing and reporting.
We all must STOP thinking like this. It FAILS us all and outcomes are not successful.
What you need to know
- Histamine intolerance is commonly associated with infections. Find them and eliminate them. Oil of Oregano, Caprylic acid and Allicin are effective at eliminating many forms of bacteria, viruses and other gut infections.
- SIBO is associated with many reasons. Fighting it with antibiotics is not the solution.
- Support stomach acid production with betaine HCl, being calm and chewing your food!
- Support bile acid production with taurine and phosphatidylcholine.
- While bile flow is being worked on, one may consider using Ox Bile to help kill infections locally in the small intestine. Use away from food before bed for best impact. Drink with a glass of water.
- Visceral manipulation is amazing for opening up your liver and gallbladder – immediately. Find a practitioner who does this. I’ve done it and works amazingly well.
- Support healthy forms of probiotics using strains which help balance histamine locally in the gut.
- Support elimination of acetylaldehyde using a multivitamin which provides all the essential components. The biggest one here is vitamin B1, Thiamine.
- It takes time. Be mindful of this and you should see continuous benefit if you are addressing it properly.
For a comprehensive article on histamine intolerance and probiotics, please review this one.
Did this answer some questions for you?!
Share them and include your experiences as well.
PS – We’re addressing histamine intolerance, gut infections, lab testing and gut repair in the Dirty Genes Summit.
Reserve your free spot today!
 800-470-7401
800-470-7401
4 Comments
I’ve been diagnosed with SIBO/Gut Dysfunction. My functional medicine doctor retired and am in the process of looking for someone to help me. I’m on numerous supplements to balance my gut and keep bacteria out of small intestine, including betaine HCI, heavy duty probiotic and GI Revive. I’m better but the SIBO has returned. I’ve narrowed it down to high histamine levels. I’ve had the StrateGene test done but can find no one to explain the results to me and provide guidance on what supplements to buy based on my results. I’m in the process of reading Dr. Lynch’s book about dirty genes. Does Dr. Lynch do any type of Zoom conferencing to go over the report with me and guide me to the proper supplements? I’m desperate!!
Dr. Lynch,
I have completed strategene testing and have MTHFR mutation. Last December I got Covid and my baby boy was still born at 38 weeks. I am now having severe histamine reactions. Is it safe to take histamine block during pregnancy? We are trying to conceive again.
Hi Christy –
Many health professionals use Histamine Block while their patients are pregnant. High histamine is associated with pregnancy complications. Consider ProBiota HistaminX in addition to Histamine Block.
Are either diatomaceous Earth or colostrum products helpful treatments to get rid of infections that cause over histamine issues?